Dual Energy X-Ray Absorptiometry in pre-obese/obese women undergoing reduction mammaplasty
Valerio Cervelli
Laura Di Renzo
Monica Grimaldi
Maria Chiara Di Fede
Pietro Gentile
Gianpiero Gravante
Nicola di Lorenzo
Antonino De Lorenzo
Reduction mammaplasty is used in order to achieve symmetric reductions in patients with asymmetries and gigantomastias. Classic techniques for the estimation of tissue to be removed are not precise, especially in patients with larger breasts and usually necessitating secondary operations for remodelling and contouring.2 A more precise estimation of the amount and location of fat, and of the remaining skin and breast tissue, would be helpful.
The Dual-Energy X-ray Absorptiometry (DEXA) is a procedure based on the three-compartment model of human composition that shows high precision in measuring the fat-mass percentage (98.8%). We conducted a prospective study with the aim to determine (1) if DEXA could be a precise technique for the assessment of the fat to be removed during surgery and (2) to evaluate, with this technique, the postoperative long-term results and changes in tissues.
Materials and methods
We prospectively enrolled all pre-obese/obese women who underwent reduction mammaplasty. We excluded patients who previously underwent bariatric surgery. Evaluation of candidates was done at the Division of Plastic and Reconstructive Surgery, University of Tor Vergata in Rome. Anthropometric parameters were measured at the Division of Human Nutrition of the same university according to standard methods (body weight, height and waist circumferences).3
The body composition was assessed by means of DEXA fan-beam scanner (Lunar model DPX-IQ, Lunar Corp., Madison).4,5 The entire body was scanned, beginning from the top of the head and moving in a rectilinear pattern towards the feet. Furthermore, the mammary region was specifically examined to evaluate the amount of fat and lean mass to be removed with surgery. Total body fat-free mass (FFM in kg), regional fat-free mass (FFM R in kg), total body fat mass (FM in kg), regional fat mass (FM R in kg), trunk body fat mass (FM T in kg) and trunk body fat free mass (FFM T in kg) were measured and recorded.
Mammary reduction was conducted according to the Planas technique.6 The patients underwent standard surgical follow-up visits, planned at the 7th, 14th and 30th postoperative day. After 6 months, they were re-examined with DEXA, recording the same parameters of the preoperative session.
Primary endpoint of the study was to assess if DEXA could be an accurate technique to estimate the composition of the breast resected. We compared the difference obtained between the preoperative and postoperative fat and lean tissue masses with the intra-operative and postoperative morphologic evaluation of tissues removed. The resected specimen was weighted during surgery, and the analysis of proportions between the fat and glandular tissues was performed later with histomorphometric correlation. Secondary endpoints were the evaluation of postoperative long-term results or changes in the total body and regional (breast) tissue distribution.
Differences between the two study groups (T0: preoperative, T1: postoperative at 6 months) were tested using the Student's t-test. Pearson's correlation index was used to evaluate the relationships among variables. All p values were considered significant if lesser than 0.05.
Results
Between 2004 and 2005 we recruited 17 pre-obese/obese women. All of them completed the study. The mean age was 43.7 10 years, height 159 6.7 cm and weight 76 7.8 kg.
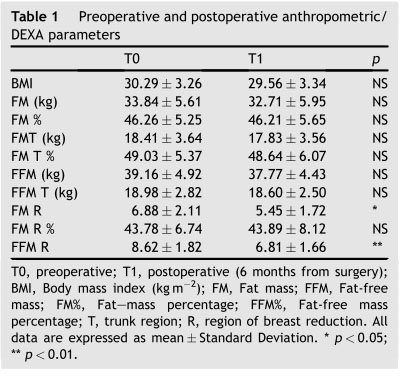
The procedure lasted 20 5 min. Maximum amount of time was required for the necessary technical adjustments before measurements could start. The anthropometric characteristics and composition values are shown in Table 1.No significant differences were observed between pre-and postoperative BMI (T0 Z 30.29 3.26 kg m-2,T1 Z 29.56 3.34 kg m-2), body weight (T0 Z 76.43 7.33 kg, T1 Z 74.57 7.97 kg), total FM (T0 Z 33.84 5.61 kg, T1 Z 32.71 5.95 kg) and FM% (T0 Z 46.26 5.25, T1 Z 46.21 5.65). Moreover, no signi?cant differences were observed in fat and fat-free mass distribution of the trunk. However, when the analysis was restricted to the breast region (R), a significant reduction of fat in kilograms (FM R, kg) after mammaplasty surgery was observed (T0 Z 6.88 2.11, T1 Z 5.45 1.72, p < 0.005). This value matched well with the intra-and postoperative
Correlations between anthropometric and DEXA parameters were performed both at T0 and T1. Interestingly, breast region fat (FM R) was positively correlated to weight (T0 coef?cient Z 0.68, p < 0.001; T1 coef?cient Z 0.62, p < 0.05; Table 2), and to FM T (T0 coef?cient Z 0.81, p < 0.001; T1 coef?cient Z 0.85, p < 0.001). Moreover, signi?cant positive correlations between FFM distributions and body weight were observed before and after surgery (Table 2).
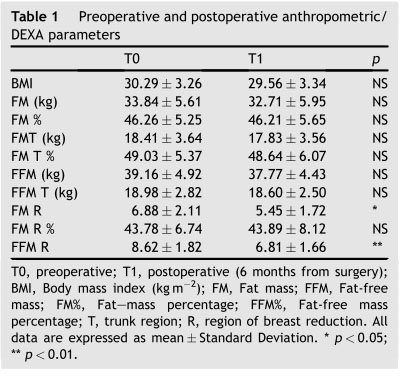
In the present study, we demonstrated that DEXA is a reliable and useful technique that assists the surgeon in the preoperative evaluation of fat and fat-free breast tissue composition in order to (1) accurately predict the amounts of fat to be removed and (2) estimate the changes in breast composition and shape after mammary reduction. The DEXA device does recognise and differentiate the human body composition of fat versus lean tissues, and such differentiation corresponds, in the breast, to the fat mass and the glandular mass. While the trunk fat-free mass values were not different between T0 and T1, a significant decrease of regional (breast) fat mass was present after surgery (p < 0.05). Intra-operative and postoperative measurements of fat removed matched perfectly with the preoperative DEXA estimation and postoperative evaluations at 6 months, confirming the accuracy of the technique. Furthermore, the weight and trunk fat masses were positively correlated to mammary fat, suggesting that surgeons should evaluate preoperatively all regions possibly affected by abnormal adipose accumulations, and not only the breast, in order to plan a correct and global patient management.
A potential flaw of this technique could be the exposure of generally well patients to an unjustifiable irradiation. However, the amount of radiation delivered by DEXA is usually extremely small e less than one-tenth the dose of a standard chest X-ray e thus minimising the exposure risks.
Our data outline the advantages of DEXA to estimate precisely the breast composition (mammary glands and fat tissue) and describe, for the first time, the changes in breast composition after the reduction mammaplasty.
Antonino De Lorenzo and Valerio Cervelli are the authors responsible for the study conception and design.
Laura Di Renzo and Gianpiero Gravante are responsible authors for data interpretation and manuscript writing.
Maria Chiara Di Fede, Pietro Gentile and Monica Grimaldi are the authors responsible for the experiment conduct. Ilaria Stazi is gratefully acknowledged for the statistical analyses and drafting of the tables and figures.
The authors do not have any financial or personal interests in any organisation sponsoring the research at the time the research was conducted.
1 Giovanoli P, Meuli-Simmen C, Meyer VE, et al. Which technique for which breast? A prospective study of different techniques of reduction mammaplasty. Br J Plast Surg 1999;52:52e9.
2 Lassus C. Breast reduction: evolution of a techniqueea single vertical scar. Aesthetic Plast Surg 1987;11:107e12.
1 Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaigne, IL: Human Kinetics; 1998.
2 De Lorenzo A, Andreoli A, Candeloro N. Within-subject variability in body composition using Dual-Energy-energy X-ray absorptiometry. Clinical Physiology 1997;17:383e4.
3 Guo Y, Franks PW, Brookshire T, et al. The intra-and inter-instrument reliability of DXA based on ex vivo soft tissue measurements. Obes Res 2004;12:1925e9.
4 Planas J, Mosely LH. Improving breast shape and symmetry in reduction mammaplasty. Ann Plast Surg 1980;4:297e303.


