Raffaele Schiavoni*, Vittorio Grenga*
* Private Practice in Orthodontics, Rome
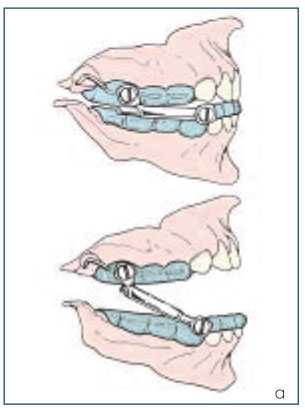
The Herbst appliance has proved to be effective in the treatment of Class II malocclusions1-22. Different methods of stabilization of the telescope mechanism have been described by different authors. The first design proposed by Pancherz in 1979 proved to be difficult both in terms of construction and clinical management because of frequent breakage23-29. One of the easiest systems of stabilization was proposed by McNamara and it consisted of upper and lower acrylic splints (Figs. 1 a-c)30-33.


Case reports
Case 1
Diagnosis and treatment plan
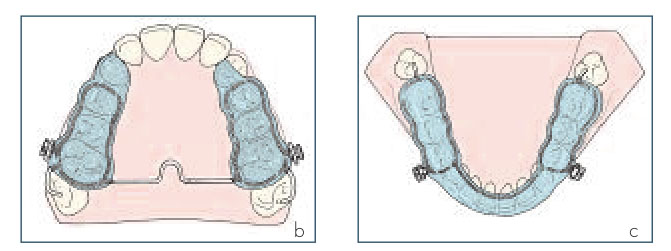
A 12-years old female presented with the chief complaint of protrusive upper incisors and difficulty in closing her lips. Clinical examination revealed a convex, retrognathic profile, lip incompetence at rest and protrusion of the upper lip. The patient had a Class II, division 1 malocclusion with an overjet of 11 mm and an overbite of 3 mm. She was in the permanent dentition with an accentuated curve of Spee and a narrow upper arch (Figs. 2 a-f). Cephalometric analysis (Fig. 3) revealed retrusion of the mandible (SNPg 70,5°) with a skeletal Class II (ANPg 5,1°). Vertical parameters showed a hyperdivergent pattern of growth (SN/Go-Gn 38,9°, Ans-Pns/Go-Gn 29,3°). The upper and lower incisors were mildly protruded (1/Ans-Pns 117,7°, 1/Go-Gn 101,7°).

1. Obtain a symmetrical Class I occlusion without extractions;
2. Improve facial appearance by stimulating mandibular growth;
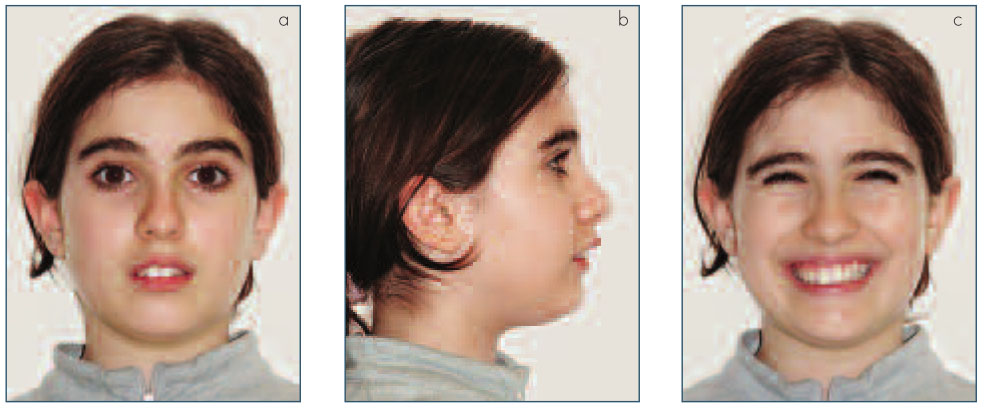
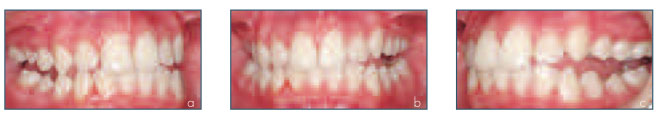
3. Avoid any extrusion of the posterior teeth of the mandible and reposition the upper incisors to allow for-nent dentition. Moreover the apward rotation of the mandible. pliance was well tolerated during meals and was never found any Treatment progress compliance problem. The appliance The first phase of treatment (9 was removed only for oral hygiene. months) involved the use of an acry-The construction bite was made with lic splint Herbst appliance. The the lower jaw protruded until the in-splints were not cemented due to cisors were edge to edge and then the possibility of maintaining good lowered to obtain a molar clearanoral hygiene and to perfect retention ce of 4-5 mm. The acrylic splints of the appliance due to the perma-were designed and built for even distribution of occlusal contacts (Figs 4 a-c). After nine months the sagittal correction was achieved and the patient presented with a posterior open bite of 3-4 mm (Figs 5 a-c). The anchorage of the Herbst appliance inhibits the dental eruption and spontaneous interocclusal setting that would normally occur. Therefore, a posterior open bite is usually present when the acrylic splints are removed. The Herbst appliance was removed and upper arch was fully bonded (.022 slot MBT prescription) and a .016 NiTi archwire was applied. The patient was instructed to wear the lower splint full time included during the meals in order to avoid the posterior shifting of the lower jaw reaching the maximum intercuspation (Figs 6 a-c). Archwire sequence of the upper arch was .016 NiTi - .019 x .025 NiTi - .019 x .025 SS. After six months the posterior open bite was closed by counterclockwise rotation of the lower jaw and the lo-wer splint was discontinued (Figs 7 a-c). At this time the lower arch was fully bonded for final alignment and coordination with the upper arch. After 22 months of treatment the patient was debonded. Two essix full coverage retainer were fitted to be worn nighttime.

Figs 6 a-c Upper arch bonded and lower splint still in place.
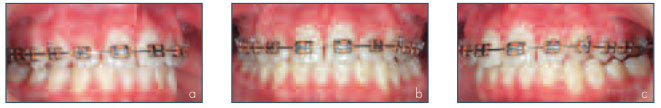
Figs 7 a-c Posterior open bite closed by counterclockwise rotation of the mandible.
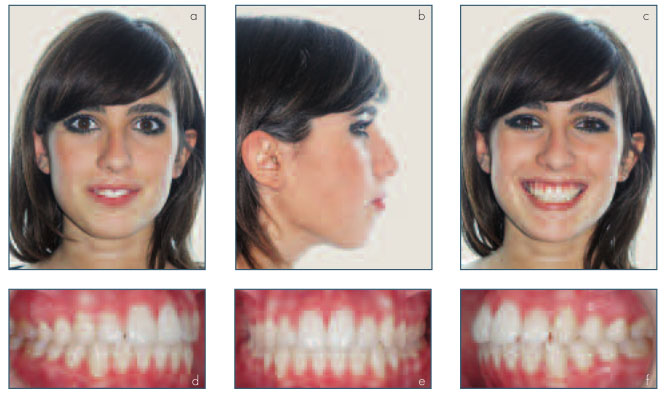
The patient?s facial appearance improved even though lip incompetence at rest was still present. Patient and her parents were totally satisfied with the result. A full Class I cuspid and molar relationship were achieved (Figs 8 a-f). Cephalometric nalysis (Fig. 9) revealed a normalization of the sagittal discrepancy (ANPg 2,8°) with control of clockwise mandibular rotation (SN/Go-Gn 38,9°, Ans-Pns/Go-Gn 26,4°). The inclination of the palatal plane increased (SN/Ans-Pns from 9,6° lower incisors were mildly proclined (1/Go-Gn from 101,7° to 109,5°) as expected in all the kinds of Herbst stabilization11,51,52.
Diagnosis and treatment plan
A 12 years old female presented with the chief complaint of crowding of upper front teeth with upper malocclusion with an overjet of 6,3 mm and an overbite of 4,6 mm. She was in permanent dentition with no crowding in the lower arch and an accentuated curve of Spee due to the infraocclusion of the posterior teeth of the lower arch (Figs 10 a-f).
Cephalometric analysis (Fig. 11) revealed a dental Class II malocclusion with no skeletal discrepancies in the sagittal plane (SNA to 12,5°) probably due to the intrusion forces produced by the telescope mechanism on the posterior segment of the upper dentition. The ramus height also increased (from 39,1 mm to 40,2 mm) in agreement with the theories of condylar displacement and growth, left cuspid out of the arch. Clinical examination revealed a convex, mild retrognathic profile with a well pronounced labiomental fold. The angle between submandibular plane and prethyroid plane (cervical angle) was accentuated.
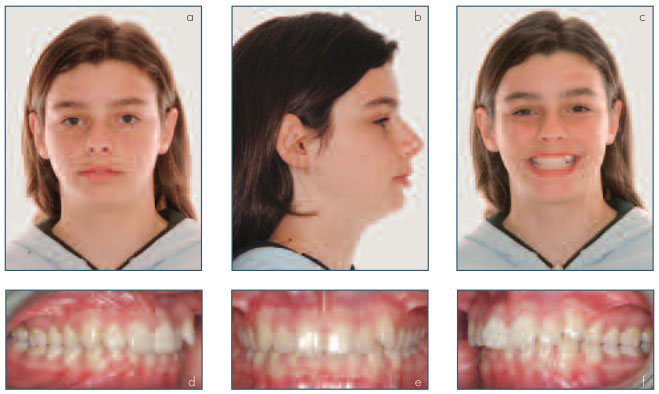
The patient had a Class II, division 1 82,2°, SNPg 77,4°). Vertical parameters showed a brachyfacial pattern of growth (SN/Go-Gn 26°, Ans-Pns/Go-Gn 17°). Lower incisors were mildly proclined (1/Go-Gn 110°).
1. Obtain a symmetrical Class I occlusion without extractions;
2. Improve facial appearance unrolling lower lip and creating a more pleasant cervical angle;
3. Allow the extrusion of the posterior lower teeth to correct the curve of Spee and to improve the overbite increasing the posterior vertical dimension.
The first phase of treatment involved the use of an acrylic Herbst appliance similar to case one both for the construction and the clinical ma-nagement (Figs 12 a-c). After nine months the sagittal correction was achieved and the patient showed a posterior open bite of 3-4 mm. The Herbst appliance was removed and upper arch was fully bonded (.022 slot MBT prescription) and a .016 Ni-Ti archwire was applied (Figs 13 a-c). Contacts were present between left and right second molars, so in the next appointment it was possible bond all the lower arch to enhance the eruption of the lower posterior teeth increasing posterior vertical dimension (Figs 14 a-c). Archwire sequence of the upper and lower arches was .016 NiTi -.019 x .025 NiTi - .019 x .025 SS. The final phase of treatment involved the use of upper and lower SS .016 arch-wires and intermaxillary elastics from upper second bicuspid to lower second molar to obtain optimal intercuspation between upper second bicuspid and the embrasure between lower second bicuspid and lower first molar (Figs 15 a-c).Total treatment time was 24 months. Two essix full coverage retainer was applied to be worn nighttime.
Treatment result
The patient ?s facial appearance improved not only for the normalization of the labio-mental fold but also for the reduction of the cervical angle. A full Class I cuspid and molar relationship was achieved (Figs 16 a-f). Cephalometric analysis (Fig. 17) revealed no significant variations in the sagittal parameters. Also in this case the palatal plane tilted backward and upward (SN/Pns-Ans from 9,1° to 10,8°) and the ramus height increased from 43,3 mm to 46 mm.




The Herbst appliance, stabilized with acrylic splints according to the McNamara design, is easy to construct, not expensive and well tolerated by the patients. The frequency of complications and the breakages of this kind of appliance are very rare when not absolutely absent. Laboratory and chair time are reduced.
For all these reasons in an orthodontic practice the management of this kind of appliance is never critical.
Moreover if the appliance is not cemented the oral hygiene is well maintained. At this stage an important key point is to induce in the patient a strong motivation to wear the appliance 24 hours per day meals included. The patient can remove the appliance only for oral hygiene. If the clinician is not sure of the patient cooperation, the appliance must be cemented. The use of the Herbst appliance stabilized with acrylic splints in different growth pattern Class II patients, induce always the same occlusal aspect at the end of Herbst phase: a posterior open bite. The next phase of treatment (posterior open bite management) can be modulated by the clinician in order to obtain better aesthetic and clinical results. In the hyperdivergent growth pattern the main goals are to reduce or better to control the vertical dimension and to induce a counterclockwise rotation of the mandible with an increase in the projection of the chin on the sagittal plane. In these cases the proclination of the upper incisors and/or the intrusion of the lower incisors together with transversal coordination of the arches allow this kind of rotation inducing the closure of the posterior open bite and minimizing the extrusion of the posterior teeth. With a normal growth pattern the main goal is to increase vertical dimension to get a lower anterior third of the face esthetically more pleasant. In these cases this can be achieved by inducing dentoalveolar vertical growth of the posterior segment and for that closing the posterior open bite and give a vertical support to the new condyledisk-ramus situation.
Conclusions
The Herbst appliance is useful in the correction of both skeletal and dental Class II malocclusions. The splint type of stabilization permits a vertical distraction of the condyle with a consequent increase of the mandible ramus length and the creation of a posterior open bite that the clinician can manage to obtain optimal results in patients with different types of growth. Unfortunately it appears to be impossible to avoid the proclination of the lower incisors confirming the difficulty to manage the incisors inclination with all types of Herbst stabilization11,51,52.
References
1 Pancherz H. Treatment of Class II malocclusions by jumping the bite with the Herbst appliance: a cephalometric investigation. Am J Orthod 1979; 76: 423-42
2 Pancherz H, Anehus-Pancherz M. Muscle activity in Class II, Division 1 malocclusions treated by bite jumping with the Herbst appliance. An electromygraphic study. Am J Orthod 1980; 78(3): 321-29.
3 Pancherz H. The effect of continuous bite jumping on the dentofacial complex: a follow-up study after Herbst appliance treatment of Class II malocclusions. Eur J Orthod 1981 Sep;3: 49-60,
4 Pancherz H, Anehus-Pancherz M. The effect of continuous bite jumping with the Herbst appliance on the masticatory system: a functional analysis of treated Class II malocclusions. Eur J Orthod 1982 Feb ; 4(1): 37-44.
5 Pancherz H. The mechanism of Class II correction in Herbst appliance treatment: a cephalometric investigation. Am J Orthod 1982; 82(2): 104-13.
6 Pancherz H. A cephalometric analysis of skeletal and dental changes contributing to class II correction in activator treatment. Am J Orthod 1984 Feb; 85(2): 125-33.
7 Pancherz H. The Herbst appliance ? Its biologic effects and clinical use. Am J Orthod 1985 Jan; 87(1): 1-20.
8 Pancherz H, Hagg U. Dentofacial orthopedics in relation to somatic maturation. An analysis of 70 consecutive cases treated with the Herbst appliance. Am J Orthod 1985 Oct; 88(4): 273-87.
10 Hagg U, Pancherz H. Dentofacial orthopaedics in relation to chronological age, growth period and skeletal development. An analysis of 72 male patients with Class II division 1 malocclusion treated with the Herbst appliance. Eur J Orthod 1986; 10: 169-76,
11 Pancherz H, Hansen K. Mandibular anchorage in Herbst treatment. Eur J Orthod 1988 May;10(2): 149-64.
12 Pancherz H, Malmgren O, Hagg U, Omblus J, Hansen K. Class II correction in Herbst and Bass therapy. Eur J Orthod 1989 Feb; 11(1): 17-30.
13 Pancherz H, Fackel U. The skeletofacial growth pattern pre- and post- dentofacial orthopaedics. A long-term study of Class II malocclusions treated with the Herbst appliance. Eur J Orthod 1990 May; 12(2): 209-18.
14 Hansen K, Pancherz H, Hagg U. Long-term effects of the Herbst appliance in relation to the treatment growth period: a cephalometric study. Eur J Orthod 1991 Dec;13(6): 471-81.
15 Hansen K, Pancherz H, Petersson A. Long-term effects of the Herbst appliance on the craniomandibular system with special reference to the TMJ. Eur J Orthod 1990 Aug;12(3): 244-53.
16 Pancherz H. The nature of Class II relapse after Herbst appliance treatment. A cephalometric long-term investigation. Am J Orthod Dentofacial Orthop 1991 Sep; 100(3): 220-33.
17 Pancherz H, Anehus-Pancherz M. The headgear effect of the Herbst appliance: a cephalometric long-term study. Am J. Orthod Dentofac Orthop 1993 Jun; 103(6): 510-19.
18 Valant Jr, Sinclair PM. Treatment effects of the Herbst appliance. Am J Orthod Dentofac Orthop 1989 Feb; 95(2): 138-47. 19 Ruf S, Pancherz H. The mechanism of Class II correction during Herbst therapy in relation to the vertical jaw base relationship: a cephalometric roentgenographic study. Angle Orthod 1997; 67(4): 271-76.
20 Ruf S, Pancherz H. The effect of Herbst appliance treatment on the manidibular plane angle: a cephalometric roentgenographic study. Am J Orthod Dentofacial Orthop 1996 Aug;110(2): 225-29.
21. Pancherz H, Michailidou C. Temporomandibular joint growth changes in hyperdivergent and hypodivergent Herbst subjects. A long term roentgenographic cephalometric study. Am J Orthod Dentofacial Orthop 2004 Aug;126(2); 153-161.
22. Bock N, Pancherz H. Herbst treatment of Class II Division 1 malocclusions in retrognathic and prognathic facial types. Angle Orthod 2006 Nov; 76(6): 930-41
23. Wieslander L. Intensive treatment of severe Class II malocclusions with a headgear-Herbst appliance in the early mixed dentition. Am J Orthod 1984 Jul; 86(1): 1-13.
24. Wieslander L. Long-term effect of treatment with the headgear-Herbst appliance in the early mixed dentition: stability or relapse? Am J Orthod Dentofac Orthop 1993 Oct; 104(4): 319-29.
25. White LW. Current Herbst aplliance therapy. Clin Orthod 1984 Aug; 28(8): 296-309.
26. Dischinger TG. Edgewise bioprogressive Herbst appliance. Clinical Orthodontics 1989; 23: 608-17
27. Berkman ME, Haerian A, McNamara JA. Interarch maxillary molar distalization appliances for Class II correction. J Clin Orthod 2008;42(1):35-42.
28. Schaefer AT, Mcnamara JA, Franchi L, Baccetti T. A cephalometric comparison of treatment with the twin block and stainless steel crown Herbst appliances followed by fixed appliance therapy. Am J Orthod Dentofacial Orthop 2004;126(1): 7-15.
29. Weschler D, Pancherz H. Efficiency of three mandibular anchorage forms treatment: a cephalometric investigation. Angle Orthod 2004; 75(1): 23-7.
30. Windmiller EC. The acrylic-splint Herbst appliance: a cephalometric evaluation. Am J Orthod Dentofacial Orthop 1993;104(1): 73-83.
31. Mcnamara JA. Jr. Fabrication of the acrylic splint Herbst appliance. Am J Orthod Dentofacial Orthop 1988;94(1):10-8.
32. Mcnamara JA. Jr, Howe RP. Clinical management of the acrylic splint Herbst appliance. Am J Orthod Dentofacial Orthop 1988;94(2): 142-9.
33. McNamara JA, Jr, Brudon WL. Orthodontic and orthopedic treatment in the mixed dentition. Needham Press, Ann Arbor, 1993. pp 263-5.
34. Voudouris JC, Kuftinec MM. Improved clinical use of twin-block and Herbst as a result of radiating viscoelastic tissue forces on the condyle and fossa in treatment and long term retention: growth relativity. Am J Orthod Dentofacial Orthop 2000;117(3); 247-66.
35. Mcnamara JA, Hinton RJ, Hoffman Dl. Histological analysis of temporomandibular joint adaptation to protrusive function in young adult rhesus monkeys (Macaca mulatta). Am J Orthod 1982;82(4): 288-98.
36. Tonge EA, Heath JK, Meikle MC. Anterior mandibular displacement and condylar growth: an experimental study in the rat. Am J Orthod 1982; 82(4): 277-87.
37. Kantomaa T. Effect of increased upward displacement of the glenoid fossa on mandibular growth. Eur J Orthod 1984 ;6(3): 183-91.
38. Woodside DG, Metaxas A, Altuna
G. The influence of functional appliance therapy on glenoid fossa remodeling. Am J Orthod Dentofacial Orthop 1987; 92(3): 181-98.
39. Tuominen M, Kantomaa T, Pirttiniemi P, Poikela A. Growth and type-II collagen expression in the glenoid fossa of the temporomandibular joint during altered loading: a study in the rat. Eur J Orthod 1996 ;18(1): 3-9.
40. Rabie AB, Zhao Z, Shen G, Hägg U, Dr O, Robinson W. Osteogenesis in the glenoid fossa in response to mandibular advancement. Am J Orthod Dentofacial Orthop 2001 ;119(4): 390-400.
41. Mcnamara JA JR, Bryan FA. Long-temp mandibular adaptations to protrusive function: An experimental study in Macaca mulatta. Am J Orthod Dentofacial Orthop 1987;92(2): 98-108.
42. Hinton RJ, Mcnamara JA. Temporal bone adaptations in response to protrusive function in juvenile and young adult rhesus monkeys. Eur J Orthod 1984;6(3):155-74.
43. Rabie AB, She TT, Hägg U. Functional appliance therapy accelerates and enhances condylar growth. Am J Orthod Dentofacial Orthop 2003;123: 40-8.
44. Rabie AB, Wong L, Tsai M. Replicating mesenchymal cells in the condyle and the glenoid fossa during mandibular forward positioning. Am J Orthod Dentofacial Orthop 2003;123(1):49-57.
45. Rabie AB, Wong L, Hägg U. Correlation of replicating cells and osteogenesis in the glenoid fossa during stepwise advancement. Am J Orthod Dentofacial Orthop 2003;123(5): 521-26.
46. Voudouris JC, Woodside DG, Altuna G, Kuftinec MM, Angelopoulos G, Bourque PJ. Condyle-fossa modifications and muscle interactions during Herbst treatment, Part 1. New technological methods. Am J Orthod Dentofacial Orthop 2003;123(6): 604-13.
47. Voudouris JC, Woodside DG, Altuna G, Kuftinec MM, Angelopoulos G, Bourque PJ. Condyle-fossa modifications and muscle interactions during Herbst treatment, Part 1. Results and conclusions. Am J Orthod Dentofacial Orthop 2003;124(1): 13-29.
48. Singh GD, Clark WJ. Localization of mandibular changes in patients with class II division 1 malocclusions treated with twin-block appliances: finite element scaling analysis. Am J Orthod Dentofacial Orthop 2001;119(4): 419-25.
49. Schiavoni R. A method used to anchor the Herbst appliance. Cranio 1988;6(3):245-51.
50. Schiavoni R, Grenga V, Macri V. Treatment of Class II high angle malocclusions with the Herbst appliance: a cephalometric investigation. Am J Orthod Dentofacial Orthop 1992;102(5): 393-409.
51. Hansen K, Theodoros G, Pancherz
H. Long-term effects of Herbst treatment on the mandibular incisor segment: a cephalometric and biometric investigation. Am J Orthod Dentofacial Orthop 1997;112(1): 92-103.
52. Ruf S, Hansen K, Pancherz H. Does orthodontic proclination of lower incisors in children and adolescents cause gingival recession Am J Orthod Dentofacial Orthop 1998;114(1):100-6.


